Rosacea is a chronic inflammatory skin condition that affects many of us, manifesting as redness, visible blood vessels, and during flare ups, acne-like pustules on the face. The condition can be both physically uncomfortable and emotionally distressing, impacting quality of life. While the exact cause of rosacea remains unknown, recent research highlights several factors that may contribute to its onset and exacerbation, including gut health, nutritional deficiencies, hormonal changes, and specific lifestyle triggers. This blog aims to explore these contributing factors in depth, offering you insights into potential underlying causes and practical strategies for managing rosacea symptoms. One of the most recent areas of research in rosacea is the link between gut health and skin conditions. The gut-skin axis suggests that imbalances in the gut microbiota can have a direct impact on skin health, potentially triggering or worsening conditions like rosacea. This connection can be underscored by the prevalence of gastrointestinal symptoms, such as bloating and discomfort, which indicate a broader systemic issue. In particular, the condition known as "leaky gut syndrome," where increased intestinal permeability allows toxins and pathogens to enter the bloodstream, has been linked to heightened inflammatory responses that manifest on the skin. The presence of Helicobacter pylori, a bacterium associated with stomach ulcers, has also been linked to rosacea in some studies. Understanding and supporting gut health can therefore be a crucial in a comprehensive rosacea management plan.
Another aspect to consider is the role of nutritional deficiencies in rosacea. Essential nutrients such as zinc, vitamin D, omega-3 fatty acids, and rutin have been identified as potentially influential in the severity and frequency of rosacea flare-ups. We explore the role of these nutrients in immune function, skin healing, overall skin barrier function and strengthening blood vessels, helping to reduce the visible signs of rosacea. Addressing these deficiencies through diet and supplementation can offer another layer of support for those managing this condition. Hormonal changes, particularly during perimenopause, can also play a significant role in the exacerbation of rosacea symptoms. The fluctuation of hormones like oestrogen can increase skin sensitivity and inflammation, making the skin more reactive to triggers. Moreover, changes in hormone levels can affect histamine metabolism, which can further exacerbate rosacea symptoms in some. Understanding these hormonal influences is essential for tailoring treatment approaches, particularly for women experiencing perimenopausal transitions.
Managing rosacea effectively often involves identifying and avoiding specific triggers that can lead to flare-ups. We will explore common food triggers, skincare products and other irritants that can exacerbate symptoms. A comprehensive approach to management, incorporating dietary adjustments, gut health support, and avoidance of known triggers, can significantly improve symptoms and quality of life for those affected. Keep reading as we delve into each of these areas in detail, providing practical guidance and evidence-based recommendations for managing rosacea.
The Gut-Skin Connection
Emerging evidence increasingly supports the notion that gut health plays a pivotal role in various skin conditions, including rosacea. This chronic inflammatory skin disorder, characterised by facial redness, visible blood vessels, and sometimes acne-like lesions, has been linked to gastrointestinal health through a mechanism known as the gut-skin axis. This connection highlights how gut dysfunction can influence skin conditions and vice versa. We delve into the gut-skin connection, focusing on leaky gut syndrome, Helicobacter pylori infections, and the role of stomach acid in rosacea. Firstly, leaky gut syndrome, also known as increased intestinal permeability, occurs when the gut lining becomes compromised, allowing larger molecules, toxins, and undigested food particles to pass into the bloodstream. This breach in the gut barrier triggers immune responses and systemic inflammation, which can manifest in various ways, including on the skin (1). In the context of rosacea, leaky gut syndrome may exacerbate symptoms by increasing inflammation. The skin and the gut share an intimate connection; they both serve as barriers and are rich in immune cells. When the gut barrier is compromised, it can lead to widespread immune activation, contributing to skin inflammation and the visible symptoms of rosacea. Supporting the gut barrier function through dietary changes, probiotics, and anti-inflammatory strategies is crucial for managing rosacea. Diets rich in fibre, fermented foods, and anti-inflammatory nutrients can help restore gut integrity and reduce systemic inflammation (2).
Several studies have suggested a potential link between Helicobacter pylori infection and rosacea. H. pylori is a bacterium that colonises the stomach lining and is primarily known for causing stomach ulcers. It can induce systemic inflammation and immune responses that may extend beyond the gastrointestinal tract, potentially exacerbating skin conditions like rosacea (3). The way H. pylori might influence rosacea involves the production of reactive oxygen species (ROS) and changes in gastric acid secretion. These changes can disrupt the gut and lead to systemic inflammatory responses. For long-term rosacea sufferers, investigating and treating H. pylori infections could alleviate symptoms, particularly if the infection is contributing to gut dysbiosis and systemic inflammation. Do speak to your GP if you are concerned about H.Pylori, who can support with testing for this.
Finally, adequate stomach acid is essential for proper digestion and nutrient absorption, particularly for minerals such as magnesium, calcium, and zinc, which are vital for skin health. Stomach acid also plays a crucial role in maintaining gut microbiota balance and preventing pathogenic bacterial overgrowth. Overuse of antacids and proton pump inhibitors (PPIs) can impair stomach acid production, leading to low stomach acid. This condition can exacerbate digestive issues, contribute to nutrient deficiencies, and alter the gut microbiota composition, increasing the risk of conditions like leaky gut syndrome (4). For those with rosacea, low stomach acid can worsen symptoms by promoting gut dysbiosis and systemic inflammation.
The gut-skin connection in rosacea highlights the importance of gut health in managing this chronic skin condition. Addressing factors such as leaky gut syndrome, H. pylori infections, and stomach acid levels can significantly impact the severity of rosacea symptoms. A comprehensive approach that includes dietary changes, probiotics, stress management, and medical intervention offers the best potential for managing rosacea effectively.
Supporting Gut Health to Manage Rosacea
To manage rosacea effectively, supporting gut health is paramount. This involves several strategies:
Dietary Interventions - Incorporating anti-inflammatory and gut-supportive foods can help. This includes a diet rich in fibre, fermented foods like yoghurt and sauerkraut, and anti-inflammatory nutrients such as omega-3 fatty acids.
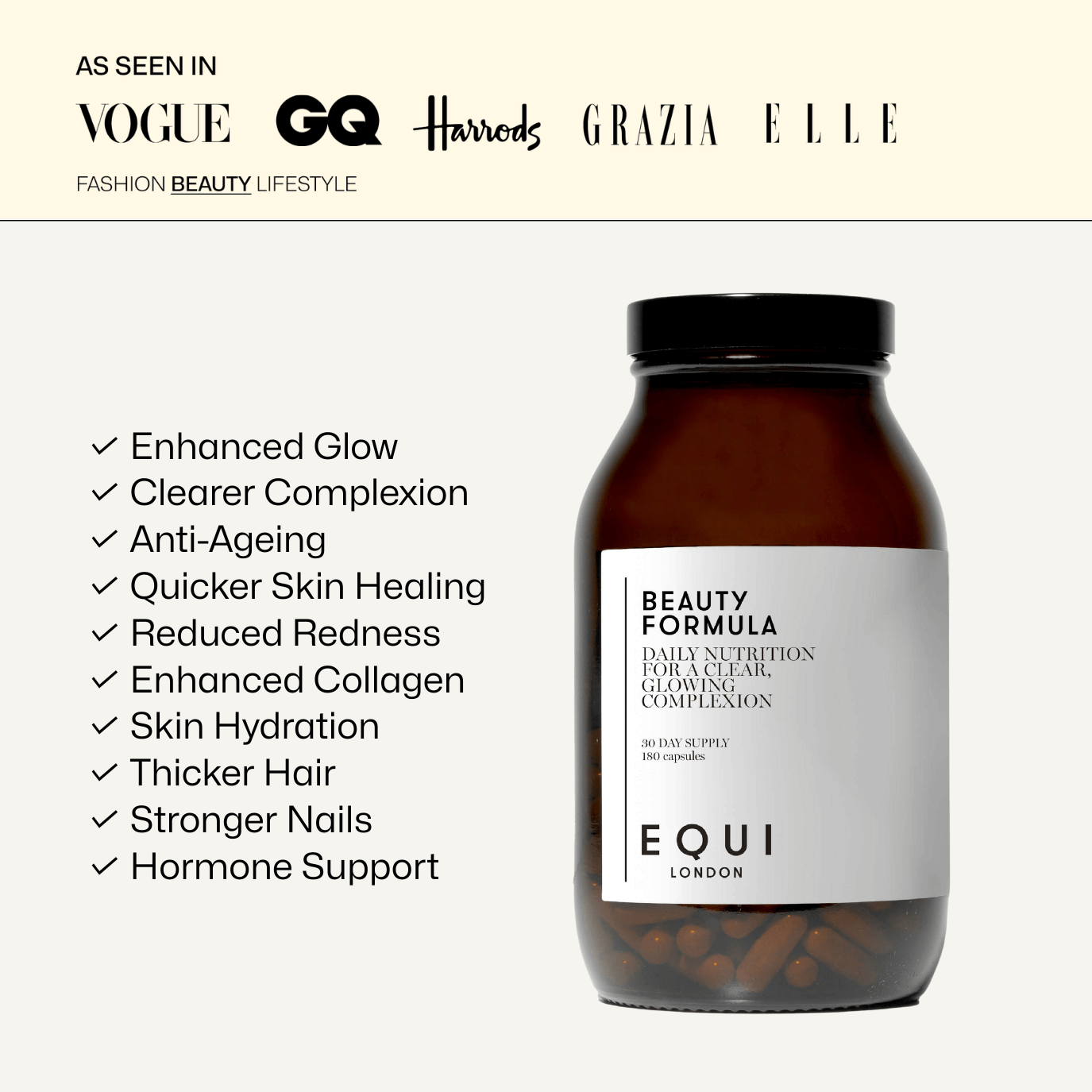
Probiotics and Prebiotics - Probiotics can help restore healthy gut microbiota balance, while prebiotics, which are non-digestible fibres, feed beneficial bacteria. We have included pre and probiotics in our best-selling Beauty Formula, which not only has a skin focus but aims to address the gut-skin axis too.
Stress Management - Chronic stress can exacerbate gut dysfunction and systemic inflammation. Stress management techniques such as mindfulness, meditation, and regular physical activity are beneficial.
Medical Evaluation - For those experiencing chronic digestive issues or suspected H. pylori infections, medical evaluation and appropriate treatment are essential. Do speak to your GP or healthcare provider if you have any gut symptoms that need addressing.
Hormonal Changes and Rosacea
While rosacea’s exact cause is unknown, various factors, including hormonal changes, can exacerbate symptoms. This is particularly evident in women undergoing perimenopause, a transitional phase leading up to menopause marked by significant hormonal fluctuations. During perimenopause, the levels of oestrogen, progesterone, and other hormones fluctuate unpredictably. Oestrogen, in particular, plays a crucial role in maintaining skin health. It helps regulate the production of sebum, a natural skin lubricant, and supports the integrity of the skin barrier. As oestrogen levels decline during perimenopause, skin becomes more susceptible to dryness, irritation, and sensitivity, all of which can exacerbate rosacea symptoms (5). Oestrogen also has anti-inflammatory properties, which help to modulate the immune response and maintain skin homeostasis. Lower oestrogen levels can lead to an increased inflammatory response, contributing to the flare-ups often seen in those with rosacea during perimenopause. This inflammatory response can result in the characteristic redness, flushing, and visible blood vessels associated with rosacea.
Histamine issues may present during perimenopause and may exacerbate rosacea symptoms. Histamine is a compound involved in local immune responses and regulating physiological functions in the gut. It can also act as a neurotransmitter. In some individuals, histamine intolerance occurs when there is an imbalance between the amount of histamine ingested and the body’s ability to break it down. This imbalance can lead to symptoms such as headaches, digestive issues, and skin reactions, including exacerbation of rosacea symptoms (6). Hormonal changes, such as those occurring during perimenopause, can influence histamine levels. Oestrogen has been shown to inhibit the activity of diamine oxidase (DAO), an enzyme responsible for degrading histamine. Lower levels of oestrogen can lead to reduced DAO activity, increasing histamine levels in the body (7). This heightened histamine level can exacerbate rosacea symptoms, as histamine can cause vasodilation, leading to flushing and redness.
Hormonal fluctuations during perimenopause can significantly impact rosacea symptoms, exacerbating skin sensitivity and inflammation. Understanding the role of oestrogen and histamine in this process is crucial for effective management. By adopting dietary changes, supporting hormonal balance, and maintaining gut health, you can better manage their symptoms and improve quality of life.
Managing Rosacea During Hormonal Changes
Managing rosacea in the context of hormonal changes involves a multi-faceted approach:
Dietary Adjustments - Reducing the intake of histamine-rich foods, such as aged cheeses, processed meats, alcohol, and certain fermented foods, can help manage symptoms. Incorporating anti-inflammatory foods and omega-3 fatty acids can also support skin health.
Hormonal Support - Consulting a healthcare professional about hormone replacement therapy (HRT) or other hormonal treatments may be beneficial for some women experiencing severe perimenopausal symptoms, including those affecting the skin.
Gut Health - Improving gut health through probiotics, prebiotics, and a balanced diet can help manage histamine levels and support overall skin health. Beauty and Menopause both have a hormonal and gut focus with pre and probiotics and key nutrients to support skin health.
Skincare - Using gentle, non-irritating skincare products and protecting the skin from environmental triggers such as extreme temperatures and sun exposure are crucial in managing rosacea symptoms.
Nutritional Deficiencies and Rosacea
Rosacea is influenced by various factors, including nutritional deficiencies. Certain nutrients are crucial for supporting the gut barrier function, immune response, and reducing inflammation, all of which can impact the severity of rosacea. For example, zinc is an essential mineral involved in many aspects of cellular metabolism, including immune function and skin health. It plays a critical role in maintaining the integrity of the skin barrier and promoting wound healing. Zinc deficiency can lead to impaired immune responses and increased inflammation, potentially exacerbating rosacea symptoms. Studies have shown that zinc supplementation can reduce inflammatory responses and improve skin conditions characterised by inflammation (8). In the context of rosacea, ensuring adequate zinc intake can help modulate the immune response and reduce inflammatory flare-ups, alleviating symptoms such as redness and pustules. In addition to zinc, vitamin D is well-known for its role in bone health, but it also possesses significant anti-inflammatory properties and is essential for maintaining skin barrier function. Low levels of vitamin D have been associated with an increased risk of various inflammatory skin conditions, including rosacea (9). Vitamin D modulates the immune system, reducing the risk of chronic inflammation. It also enhances the production of antimicrobial peptides in the skin, which can protect against infections and inflammation. Supplementation with vitamin D may be a potential strategy to help manage rosacea by reducing inflammation and supporting overall skin health.
Omega-3 fatty acids, primarily found in fatty fish such as salmon, mackerel, and flaxseeds, have potent anti-inflammatory effects. These fatty acids are crucial components of cell membranes and play a significant role in inflammatory processes. Omega-3s, particularly EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), can help reduce the production of pro-inflammatory cytokines, mitigating the inflammatory response associated with rosacea (10). Increasing the intake of omega-3 fatty acids through diet or supplements can help reduce the frequency and severity of rosacea flare-ups, promoting a calmer skin appearance. Finally, rutin, a bioflavonoid found in foods such as buckwheat, apples, and citrus fruits, has strong antioxidant properties. It is known to strengthen blood vessels and reduce capillary fragility, which is particularly relevant for rosacea sufferers who experience visible blood vessels and flushing (11). By strengthening the vascular structure, rutin can help reduce the visibility of blood vessels and the occurrence of flushing. Its antioxidant properties also contribute to reducing oxidative stress and inflammation, further supporting skin health.
Nutritional deficiencies can play a significant role in the development and exacerbation of rosacea symptoms. Ensuring adequate intake of zinc, vitamin D, omega-3 fatty acids, and rutin can help support immune function, maintain skin barrier integrity, and reduce inflammation. For those with rosacea, addressing these deficiencies through diet and supplementation offers a practical approach to managing and alleviating symptoms. We created Beauty Formula to support a wide range of skin conditions including rosacea. It contains a blend of over 45 highly effective nutritional compounds designed to target problem skin and brighten all complexions, while also nourishing, energising, and balancing the whole body. Meanwhile, Beauty Oil Edition is the first beauty-specific omega 3 supplement, to support brightness, hydration, reduce inflammation and overall heath. Shop Total Beauty here.
Identifying Triggers and Avoiding Flare-Ups
Rosacea is a chronic skin condition that can be exacerbated by various environmental, dietary, and lifestyle factors. Identifying and avoiding these triggers is crucial for managing symptoms and preventing flare-ups. This article explores common triggers, problematic skincare products, and strategies for managing and avoiding triggers to maintain clearer, healthier skin. Rosacea flare-ups can be triggered by a range of factors, including certain foods, drinks, and environmental conditions. Some of the most common dietary triggers include:
Alcohol - Consuming alcohol, particularly red wine, is a well-known trigger for rosacea. Alcohol causes vasodilation, which can lead to increased redness and flushing (12).
Spicy Foods - Foods containing capsaicin, such as hot peppers, can exacerbate rosacea symptoms by causing flushing and redness.
Hot Beverages - Consuming hot drinks like coffee and tea can trigger flushing in some individuals with rosacea.
Histamine-Rich Foods - Foods high in histamines, including aged cheeses, processed meats, and fermented products, can worsen rosacea symptoms. Histamines cause blood vessels to dilate, leading to increased redness and flushing (13).
Problematic Skincare Products
Certain skincare ingredients can irritate sensitive, rosacea-prone skin, leading to flare-ups. Key irritants include:
Alcohol and Fragrance - These ingredients are common in skincare products and can strip the skin of its natural oils, leading to irritation and dryness. Fragrances, both synthetic and natural, can be particularly irritating.
Vitamin C Serums - While beneficial for some skin types, high concentrations of vitamin C can be irritating for those with rosacea, leading to increased redness and sensitivity (14).
Essential Oils - Some essential oils, such as eucalyptus and peppermint, can irritate the skin and exacerbate rosacea symptoms.
LED Lights - Although LED treatments are generally considered safe, some individuals with rosacea may find that LED lights, especially blue light, can worsen their symptoms due to increased sensitivity (15).
Managing Triggers
Effectively managing rosacea involves identifying and avoiding personal triggers. One of the most effective ways to do this is by keeping a symptom diary. This diary should include:
Daily Activities - Note any foods, drinks, skincare products, or environmental exposures.
Symptoms - Record any changes in skin condition, such as increased redness, swelling, or the appearance of new pustules.
External Factors - Consider weather conditions, stress levels, and other external factors that may contribute to flare-ups.
By analysing this diary over time, you may be able to identify patterns and pinpoint specific triggers. This knowledge allows for more effective management strategies, such as adjusting diet, skincare routines, or lifestyle habits to avoid these triggers.
Managing rosacea requires a proactive approach to identifying and avoiding triggers that can exacerbate symptoms. Common dietary triggers include alcohol, spicy foods, hot beverages, and histamine-rich foods. Problematic skincare products containing alcohol, fragrance, and certain active ingredients can also contribute to flare-ups. By keeping a symptom diary and closely monitoring their skin's response to various factors, individuals can develop a tailored approach to managing their rosacea, reducing the frequency and severity of flare-ups.
Disclaimer: All of the information on this website is provided for general information only, it should not be treated as a substitute for the medical advice of your own doctor or any other health care professional providing personalised nutrition or lifestyle advice. If you have any concerns about your general health, you should contact your local health care provider. No one diet or supplement regime works for everyone and you should always seek help from a GP and registered health expert before making changes to your diet, or before introducing any supplements. This is especially important when pregnant.
References
- Fasano, A. (2012). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology, 42(1), 71-78.
- Bischoff, S. C., Barbara, G., Buurman, W., Ockhuizen, T., Schulzke, J. D., Serino, M., ... & Wells, J. M. (2014). Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterology, 14(1), 189
- Gravina, A. G., Federico, A., Ruocco, E., Lo Schiavo, A., Masarone, M., Tuccillo, C., ... & Romano, M. (2015). Helicobacter pylori infection but not small intestinal bacterial overgrowth may play a pathogenic role in rosacea. United European Gastroenterology Journal, 3(1), 17-24.
- Reimer, C. (2013). Safety of long-term PPI therapy. Best Practice & Research Clinical Gastroenterology, 27(3), 443-454.
- Brincat, M., et al. (20024). Menopause and The Effects of Hormone Replacement Therapy on Skin Aging. Gynecological and Reproductive Endocrinology and Metabolism, 5 (1), pp.34-37
- Maintz, L., & Novak, N. (2007). Histamine and Histamine Intolerance. The American Journal of Clinical Nutrition, 85(5), 1185-1196.
- Sanchez-Perez et al. (2022). The Rate of Histamine Degradation by Diamine Oxidase Is Compromised by Other Biogenic Amines. Frontiers in Nutrition, 9.
- Ogawa, Y., Kawamura, T., Shimada, S., & Nishida, E. (2018). Zinc and skin disorders. Nutrients, 10(2), p. 199.
- Mostafa WZ, Hegazy RA. Vitamin D and the skin: Focus on a complex relationship: A review. J Adv Res. 2015 Nov;6(6):793-804.
- Calder, P. C. (2013). Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? British Journal of Clinical Pharmacology, 75(3), 645-662.
- Gęgotek A, Rybałtowska-Kawałko P, Skrzydlewska E. (2017). Rutin as a Mediator of Lipid Metabolism and Cellular Signaling Pathways Interactions in Fibroblasts Altered by UVA and UVB Radiation. Oxid Med Cell Longev. 4721352.
- Wilkin, J., Dahl, M., Detmar, M., Drake, L., Liang, M. H., Odom, R., ... & National Rosacea Society Expert Committee. (2002). Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. Journal of the American Academy of Dermatology, 46(4), pp. 584-587.
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American Journal of Clinical Nutrition, 85(5), pp. 1185-1196.
- Del Rosso, J. Q., & Levin, J. (2011). The clinical relevance of maintaining the integrity of the stratum corneum in the treatment of patients with rosacea: the role of skin care and cosmeceuticals. Journal of Drugs in Dermatology, 4 (9), pp. 22-42.
- Goldberg, D. J. (2012). Current trends in intense pulsed light. Journal of Clinical and Aesthetic Dermatology, 18(3), pp. 45-53