Oestrogen dominance, low progesterone, high androgens.. what do all of these mean, do they apply to you and what can we do to keep our hormone balanced?
Most women will know just how strongly our hormones govern how we feel on a day-to-day basis – mood, energy, digestion, skin and sleep can all be impacted on by what time of the month it is. To some extent this is normal (we encourage you to check out this article on Cycle Synching to encourage you to stay in tune with yours) but if the impacts are becoming difficult to manage or if you experience PMS, have diagnosed hormonal conditions or regularly need medications such as pain killers, then you may be interested to know that there are many things you can do to help you manage this.
This week we have Registered Nutritional Therapist and Women’s health specialist Jen Walpole offering her insights into the signs, symptoms and conditions associated with hormone imbalances and what we can do to balance our hormones naturally.
(The first half of this article expands on hormone health, and the second outlines what you can do to manage hormone balance. If you don’t want the more sciencey detail, scroll down to the second half for our tips!)
The Basics
Hormones are ‘chemical messengers’ secreted by endocrine glands to regulate physiology, behaviour and the ability to reproduce. The sex hormones are steroid hormones produced primarily by the ovaries. Other endocrine glands are involved in the production of sex hormones including the hypothalamus and pituitary glands in the brain, which trigger production. The sex hormones (and by that we don’t just mean things that boost libido, but instead those that control our reproductive and fertility systems) can be classed as androgens, oestrogens, and progesterone’s. We also produce gonadotropin-releasing hormone (GnRH), luteinising hormone (LH) and follicle stimulating hormone (FSH), which play a role in the menstrual cycle. The hypothalamus secretes GnRH to stimulate the pituitary gland to produce LH and FSH, which triggers sex hormone production. The process itself is complex and requires a series of events as well as a particular environment to function efficiently and support hormone balance. Whilst androgens (such as testosterone) are regarded as the ‘male’ sex hormones, they do play an important role in women too. Beyond their role in the menstrual cycle and reproduction, the sex hormones are also involved in bone density (1), skin integrity, energy (2), mood, cognition (3), and vascular function (4).
The Menstrual Cycle
All of these hormones naturally fluctuate throughout the course of the monthly cycle as the ovaries prepare for ovulation and the uterus develops a thick endometrium in readiness for potential fertilisation. The follicular phase of the cycle is characterised by a rise in oestrogen and FSH, stimulating the development of follicles (folliculogenesis). One follicle will reach maturity, containing an egg, which is released when a drop in oestrogen alongside a peak in LH and FSH triggers ovulation. LH and FSH will cause the remaining dominant follicle to transform into the corpus luteum, which produces progesterone. This post-ovulation phase is known as the luteal phase as progesterone prepares the uterus to facilitate implantation in the event of fertilisation. During most of the luteal phase, oestrogen will also remain relatively high to help progesterone thicken and maintain the lining. When fertilisation does not occur, progesterone levels fall, triggering menstruation and the beginning of the next cycle.
Hormone Balance
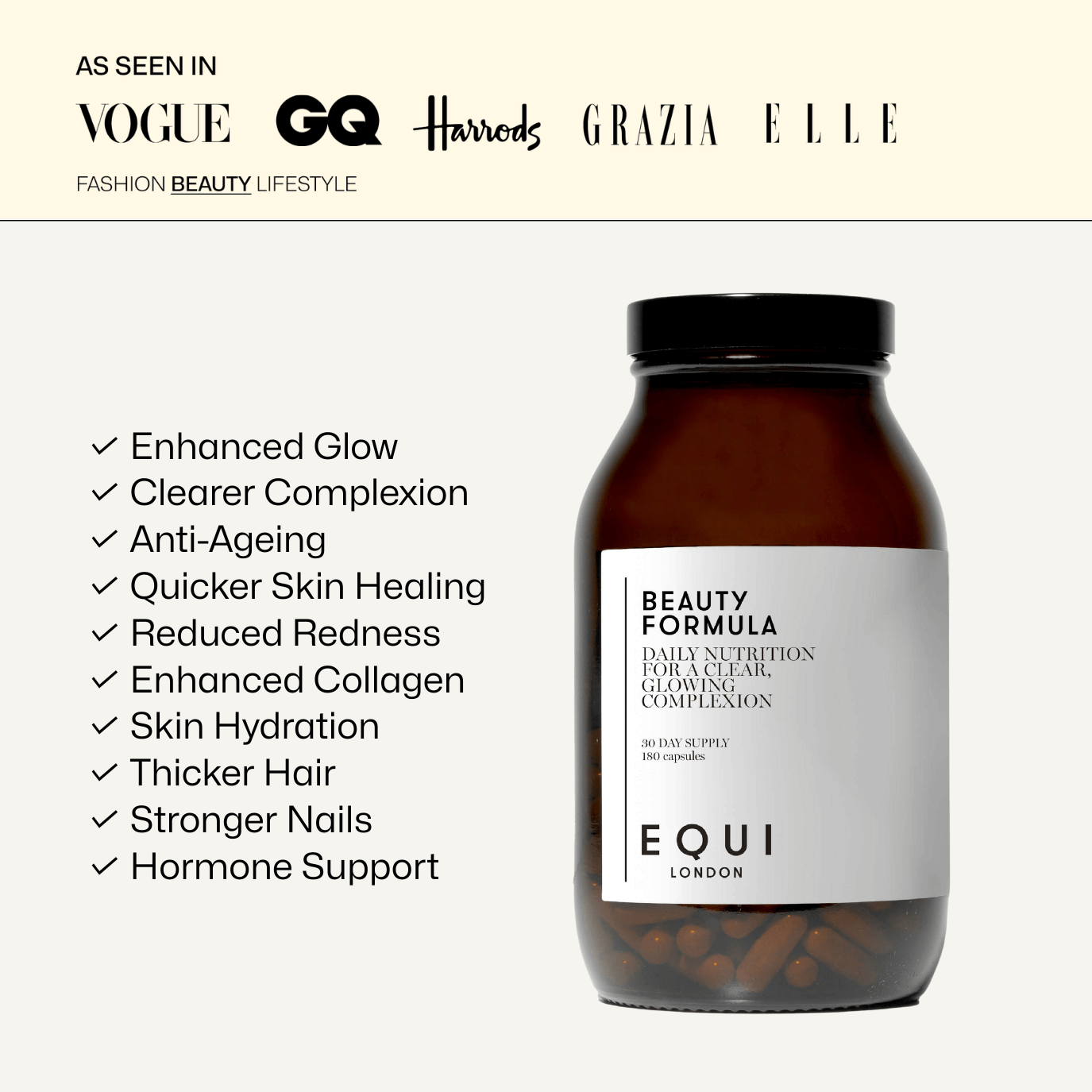
Equi believes that wellbeing comes from living in a state of balance – be in your daily lifestyle, or balance internally throughout all your body systems.
The menstrual cycle is no different and relies totally on hormone balance. This is tightly regulated, like many processes in the body (5). Hormone balance is as much about the production and transportations of hormones, as it is their elimination via detoxification and the gut. Despite the fact the body tightly regulates this process, there are many factors which can disrupt hormone balance and dysregulate the menstrual cycle. For example, blood sugar dysregulation, constipation, obesity or low body weight and chronic stress.
Let’s have a look at some of the key scenarios that may be responsible for hormone imbalances.
High Oestrogen
Typical symptoms and conditions in women associated with elevated oestrogen, or so-called 'oestrogen dominance' include premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) (6), heavy and/or painful periods, water retention (7), fibroids (8), endometriosis (9), fibrocystic breasts (10) and regular, monthly headaches or migraines (11). Inflammatory markers have also been identified in women with PMS (12).
But what is the process that drives high oestrogen in the first place? You may have come across the term ‘oestrogen dominance’ before however, there is much more to this process than the term suggests. For example, excess insulin (due to diet and bloody sugar dysregulation) can drive higher levels of testosterone and oestrogen through a process known as ‘aromatisation’. This process can be increased further in women with high cortisol levels (cortisol is the stress hormone).
Environmental factors may also drive excess oestrogen such as exposure to xeno-estrogens, which are synthetic oestrogens present in everyday items such as plastics, parabens, aluminium (including anti-perspirants) and heavy metals such as mercury or pesticides. Poor elimination by way of detoxification and the gut can lead to recirculating and potentially, excess oestrogen. Therefore, we can see it’s not as simple as producing too much oestrogen – there are many more drivers to consider!
Low Oestrogen
On the opposite end of the scale, some women present with low oestrogen. Typically, this is due to the menopause, however, for some, this can happen during the reproductive years. Signs and symptoms include irregular periods (13), annovulation (no egg is released) (14), amenorrhea (absence of periods during the reproductive years) (15), infertility, low libido, osteopenia/osteoporosis, poor skin integrity and elasticity, low mood, depression and/or the depressive form of PMS (16), dull or dry hair and/or hair loss, fatigue and impaired memory and concentration.
The main driver for low oestrogen during the reproductive years is low body fat percentage alongside chronic high cortisol (stress). In particular, a diet restrictive of fats and carbohydrates impairs the ability of the body to produce enough cholesterol, which is needed to make the sex hormones. Extreme weight loss may reduce the conversion of testosterone into oestrogen (via aromatisation), contributing to low levels of oestrogen. Chronic stress and disrupted sleep can deplete the production of the sex hormones and may drive something known as hypothalamic amenorrhoea, which is a common form of amenorrhoea resulting in oestrogen deficiency (17). Another possible driver of low oestrogen is chronic mal-digestion and malabsorption, particularly of fat, which is needed to produce the sex hormones. Those with Chronic digestive conditions such as inflammatory bowel disease (IBD) or dysbiosis are more prone to macro and micro-nutrient insufficiencies.
High Androgens
High androgens such as testosterone (the major androgen in women) are most associated with PCOS, alongside an elevated LH:FSH ratio. Otherwise known as hyper-androgenism, signs and symptoms include hirsutism (male pattern hair growth in women), acne (18), irregular periods (19), annovulation (20), angry/irritable PMS or PMDD, polycystic ovaries and infertility (21). PCOS is a common syndrome, affecting up to 1 in 10 women (22) and a major driver of anovulatory infertility. Closely associated with insulin resistance, women that have PCOS may find it harder to lose weight due to disrupted blood/glucose regulation. Elevated insulin/insulin resistance in turn reduces a transport hormone protein known as sex hormone binding globulin (SHBG), which increases testosterone levels further. As in high oestrogens, high androgens may be driven by poor elimination, which means the liver (detoxification) and the gut must be considered in this picture too.
Low Androgens
Low testosterone in women during the reproductive years is less common. Some of the signs and symptoms include fatigue, sleep disturbances, reduced libido (23), irregular menstrual cycles (24), vaginal dryness, and muscle weakness. Testosterone levels naturally decline with age due to the menopause. During the reproductive years, a common cause can be a low body fat percentage, as seen in low oestrogen. For example, a low fat/low calorie diet or severe digestive issues leading to low micro/macro nutrient intake may impair testosterone production.
How To Support Hormone Balance Naturally
Now, we have a better understanding of the key scenarios of hormone imbalances, what can we do to support hormone balance naturally? Here are top 5 achievable ways to support general hormone balance through nutrition and lifestyle hints and tips.
1. Blood Sugar Balance
As mentioned, insulin resistance can drive symptoms of hormone imbalances and so working on balancing blood sugar levels is key. Good quality carbohydrates are essential for hormone balance, but it is important to distinguish those ‘good’ ones from carbohydrates that can drive blood sugar imbalances. For example, wholegrains would be a fantastic choice compared to white grains. Processed carbohydrates, which are often high in saturated fat as well as refined sugar should be avoided or kept to a minimum such as cakes, sweets, and biscuits. This also includes natural sweet treats which are usually marketed as healthy options. Choosing mostly low GL foods is a good strategy, which means going for brown rice, buckwheat, rye, berries, apples, citrus fruits, and bananas instead of white rice/pasta/bread and dried fruits. It is a good idea to add protein to every meal and snack (meat, fish, eggs, nuts, seeds, lentils, pulses) to keep blood sugar stable.
Magnesium intake is associated with better blood sugar balance (25) as is lesser-known mineral manganese (26).
2. Maintain a healthy BMI
Whilst BMI is a confusing marker of health, in relation to hormone balance, it can be helpful to monitor. A BMI of between 20-25 is ideal to support hormone balance as we have seen being both underweight and obese can have equally detrimental effects to hormone production (27). If overweight, it’s important not to lose weight too drastically, which can increase cortisol levels and down regulate the sex hormones. Losing weight will also help reduce inflammatory markers, which can be seen in women with bad PMS.
For women that are underweight, it’s important to firstly establish what may be driving this and support accordingly. Increasing fat and carbohydrate intake will help support the return of the menstrual cycle. For anyone out there struggling with an eating disorder, consult your GP for support or see Mind’s list of contacts for help.
3. Improve Detoxification & Digestion
Detoxification is required to eliminate ‘used’ hormones and optimal digestion helps supply the body with the key nutrients needed for hormone production and balance. Alcohol consumption is negatively associated with hormone balance due to the role it plays in impairing detoxification (28) so it is a good idea to limit your consumption to the UK government’s recommended levels of 14 units per week.
Bitter foods not only help aid the digestion of the fats needed to produce hormones, but they also support detoxification. Cruciferous vegetables such as kale, broccoli, cabbage and bitters including rocket, watercress and chicory should be eaten regularly to support hormone balance. These foods are also rich in B vitamins, which are necessary for hormone balance, one of the reasons why we add highly bio-available, active B-complex into each of Equi's Formula range.
A diet rich in fibre plays an important role in supporting a healthy and diverse microbiome which is vital for helping to keep the gut moving daily – one of the most important things you can do to balance your hormones. Prebiotic-rich foods such as garlic, leeks, Jerusalem artichokes and bananas help feed the beneficial bacteria in the gut whilst probiotic-rich foods such as kefir, kimchi, sauerkraut, and miso help inoculate the gut with friendly bacteria which is important for hormone regulation.
4. Reduce Stress & Improve Sleep
The sleep/wake cycle, known as the circadian rhythm, is often dysregulated in women that struggle with hormone imbalances. Establishing a good sleep routine, with regular bedtimes/wake times, at least 7-8 hours sleep per night, sunlight exposure during the day whilst limiting exposure to blue light in the evening are helpful strategies to improving sleep and supporting hormone balance. Reducing stimulants such as caffeine is also key. Practicing mindfulness techniques such as meditation, breathwork or journaling may help to reduce daily life stressors. Antioxidant vitamin C play a role in the reduction of cortisol levels (29). Some herbs that might be helpful to reduce stress include ashwagandha, schisandra, Siberian ginseng, lavender (30) and lemon balm (31).
Knowing that in the modern world, no matter how hard we try to avoid it, women are still sometimes exposed to stress, sleeplessness and anxiety, we include a blend of minerals, vitamins and botanicals in all Equi Formula’s to help with adrenal function.
5. Reduce Exposure to Endocrine Disruptors
As mentioned, environmental toxins can disrupt hormone balance. Making the switch to natural products, limiting plastic consumption (don’t microwave in plastic or wrap food in cling film and try to use plastic free drinking bottles and cups) choosing organic food and products as well as reducing exposure to pollution are all easy strategies that can help support hormone balance.
References
- Ho-Pham, L.T. Nguyen, N.D. & Nguyen, T.V. (2013). ‘Quantification of the relative contribution of estrogen to bone mineral density in men and women’. BMC Musculoskeletal Disorders,14, p. 366.
- Mauvais-Jarvis, F. Clegg, D.J. Hevener, A.L. (2013). ‘The Role of Estrogens in Control of Energy Balance and Glucose Homeostasis’, Endocrine Reviews, 34 (3), pp. 309–338.
- Gurvich, C. Hoy, K. Thomas, N. and Kulkarni, J. (2018). ‘Sex Differences and the Influence of Sex Hormones on Cognition through Adulthood and the Aging Process’. Brain Sciences, 8 (9), p.163.
- Khalil, R. (2005). ‘Sex Hormones as Potential Modulators of Vascular Function in Hypertension’. Hypertension, 46 (2), pp. 249-254.
- Schmalenberger, K. Tauseef, H. Barone, J. Owens, S. Lieberman, L. Jarczok, M. Girdler, S. Kiesner, J. Ditzen, B. and Eisenlohr-Moul, T. (2021). ‘How to study the menstrual cycle: Practical tools and recommendations’. Psychoneuroendocrinology, 123, p. 104895.
- Toffoletto, S. Lanzenberger, R. Gingnell, M. Sundström-Poromaa, I. and Comasco, E. (2014). ‘Emotional and cognitive functional imaging of estrogen and progesterone effects in the female human brain: A systematic review’. Psychoneuroendocrinology, 50, pp.28-52.
- Stachenfeld, N. (2008). ‘Sex Hormone Effects on Body Fluid Regulation’. Exercise and Sport Sciences Reviews, 36 (3), pp.152-159.
- Bulun, S. (2013). ‘Uterine Fibroids’. New England Journal of Medicine, 369 (14), pp.1344-1355.
- Vercellini, P. Viganò, P. Somigliana, E. and Fedele, L. (2013). ‘Endometriosis: pathogenesis and treatment’. Nature Reviews Endocrinology, 10 (5), pp. 261-275.
- Wypych, K. Kuźlik, R. Wypych, P. Zaburzenia. (2002). ‘hormonalne u kobiet z makrotorbielami gruczołów sutkowych [Hormonal abnormalities in women with breast cysts]’. Ginekol Pol. 73 (11), pp. 1117-25.
- Borsook, D. Erpelding, N. Lebel, A. Linnman, C. Veggeberg, R. Grant, P. E. Buettner, C. Becerra, L. & Burstein, R. (2014). ‘Sex and the migraine brain’. Neurobiology of disease, 68, pp. 200–214.
- Berton-Johnson, E.R. (2014). ‘Association of inflammation markers with menstrual symptom severity and premenstrual syndrome in young women’ Human Reproduction. 29 (9), pp. 1987-1994.
- Farland, L. V. Mu, F. Eliassen, A. H. Hankinson, S. E. Tworoger, S. S. Barbieri, R. L. Dowsett, M. Pollak, M. N. & Missmer, S. A. (2017). ‘Menstrual cycle characteristics and steroid hormone, prolactin, and growth factor levels in premenopausal women’. Cancer causes & control, 28 (12), pp. 1441–1452.
- Hambridge, H.L, Mumford, S.L. Mattison, D.R. Ye, A. Pollack, A.Z. Bloom, M.S. Mendola, P. Lynch, K.L. Wactawski-Wende, J. Schisterman, E.F. (2013). ‘The influence of sporadic anovulation on hormone levels in ovulatory cycles’, Human Reproduction, 28 (6), pp. 1687–1694.
- Meczekalski, B. Katulski, K. Czyzyk, A. (2014). ‘Functional hypothalamic amenorrhea and its influence on women’s health’. Journal of Endocrinology Investigation37, pp. 1049–1056.
- Lei, R. Sun, Y. Liao, J. Yuan, Y. Sun, L. Liu, Y. Yang, X. Ma, W. and Yu, Z. (2021). ‘Sex hormone levels in females of different ages suffering from depression’. BMC Women's Health, 21(1).
- Torbati, T. Dutra, E. and Shufelt, C. (2017). ‘Hypothalamic Amenorrhea and the Long-Term Health Consequences’. Seminars in Reproductive Medicine, 35 (03), pp. 256-262.
- Arora, M. Yadav, A. and Saini, V. (2011). ‘Role of hormones in acne vulgaris’. Clinical Biochemistry, 44 (13), pp.1035-1040.
- Karrer-Voegeli S, Rey F, Reymond MJ, Meuwly JY, Gaillard RC, Gomez F. (2009). ‘Androgen dependence of hirsutism, acne, and alopecia in women: retrospective analysis of 228 patients investigated for hyperandrogenism’. Medicine (Baltimore), 88(1), pp.32-45.
- Norman, R. Dewailly, D. Legro, R. and Hickey, T. (2007). ‘Polycystic ovary syndrome’. The Lancet, 370 (9588), pp.685-697.
- Wu, S. Divall, S. Nwaopara, A. Radovick, S. Wondisford, F. Ko, C. & Wolfe, A. (2014). ‘Obesity-induced infertility and hyperandrogenism are corrected by deletion of the insulin receptor in the ovarian theca cell’, Diabetes, 63(4), pp.1270–1282.
- Mousa, S. Brady, Mousa, S. and Mousa, (2009). ‘Polycystic ovary syndrome and its impact on women & quality of life: More than just an endocrine disorder’. Drug, Healthcare and Patient Safety, p.9.
- Basson R. (2010). ‘Testosterone therapy for reduced libido in women’. Therapeutic advances in endocrinology and metabolism, 1(4), pp.155–164.
- Van Anders, S. and Watson, N. (2006). ‘Menstrual cycle irregularities are associated with testosterone levels in healthy premenopausal women’. American Journal of Human Biology, 18 (6), pp.841-844.
- Rumawas, M. McKeown, N. Rogers, G. Meigs, J. Wilson, P. and Jacques, P. (2006). ‘Magnesium Intake Is Related to Improved Insulin Homeostasis in the Framingham Offspring Cohort’. Journal of the American College of Nutrition, 25(6), pp.486-492.
- Du, S. Wu, X. Han, T. Duan, W. Liu, L.Qi, J. Niu, Y. Na, L. and Sun, C. (2018). ‘Dietary manganese and type 2 diabetes mellitus: two prospective cohort studies in China’. Diabetologia, 61(9), pp.1985-1995.
- Ziomkiewicz, A. Ellison, P.T. Lipson, S.F. Thune, I. Jasienska, G. (2008). ‘Body fat, energy balance and estradiol levels: a study based on hormonal profiles from complete menstrual cycles’, Human Reproduction, 23(11), pp. 2555–2563
- Erol, A. Ho, A. Winham, S. and Karpyak, V. (2017). ‘Sex hormones in alcohol consumption: a systematic review of evidence’. Addiction Biology, 24(2), pp.157-169.
- Brody, S. Preut, R. Schommer, K. (2002). ‘A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress’. Psychopharmacology,159, pp. 319–324.
- Fißler, M. and Quante, A. (2014). ‘A case series on the use of lavendula oil capsules in patients suffering from major depressive disorder and symptoms of psychomotor agitation, insomnia and anxiety’. Complementary Therapies in Medicine, 22(1), pp.63-69.
- Cases, J. Ibarra, A. Feuillère, N. Roller, M. and Sukkar, S. (2010). ‘Pilot trial of Melissa officinalis L. leaf extract in the treatment of volunteers suffering from mild-to-moderate anxiety disorders and sleep disturbances’. Mediterranean Journal of Nutrition and Metabolism, 4(3), pp.211-218.
Disclaimer: Certain supplements are used for different reasons and a one-size-fits-all approach shouldn’t be adopted. In addition, pregnant women and anyone on medication should always consult a doctor before embarking on a supplements programme. As with all articles on www.equilondon.com, this is no substitution for individual medical or nutritional advice.