Is my gut causing acne, eczema, rosacea or psoriasis?
If you’ve got a skin issue, then the chances are you’ve spent a lot of time wondering what’s causing it...
A new washing powder or face wash, something you’re breathing in, or perhaps a new intolerance to food such as dairy or gluten are all things we immediately question when issues develop. If the problem is persistent, you may have gone to huge lengths to work out what to do – cutting out sugar, doing a detox, or even starting a new medication or steroid cream. The problem is that many of these things don’t get to the heart of the issue that is underlying your skin issue, and more and more research is showing that supporting our gut could be the answer to our problems. Let us explain why..
What is the gut skin-axis?
We’ve become familiar with the gut-brain axis, but have you ever taken a moment to consider the gut-skin axis? With more and more evolving research into the impact of our gut microbiome for our overall health and wellbeing – do the microbes that live in our digestive tract also have an impact on the appearance of our skin?
The human microbiome plays a key role in regulating the immune system within the body, since it communicates with tissues and organs in a direct way maintain homeostasis (balance) within the body. With this in mind, it seems that imbalanced gut bacteria in the either the skin’s microbiome (that’s right – just like the gut, it has its own) or gut microbiome can over time lead to altered immune responses, promoting topical issues such as dermatitis/eczema, psoriasis, acne vulgaris, dandruff, and possibly even skin cancer. (4)
Despite how common skin conditions can be, conventional treatments such as medications or topical remedies remain only partially beneficial – covering the symptom rather than understanding the root cause – and you may know by now that at Equi, we’re all about getting to the root at the problem!
Hormonal acne and the gut
Acne is an inflammatory skin condition that we often tally up with teenage years of puberty and raging hormones – we remember those days, right? Well forget what you think you know, acne can flare up as basically any age – 20’s, 30’s, 40s and even during perimenopause.
Whilst hormonal fluctuations can have a significant impact on sebum regulation of the skin, many inflammatory skin conditions have also been directly linked to imbalances within the gut microbiome. When excess skin cells line the inside of hair follicles, sebum cannot be excreted, causing acne. As a result, bacteria are allowed to grow, triggering an inflammatory response from your immune system. Why is this significant for acne? Because over 70% of our immune cells are created and located in your gut, and the gut bacteria is central to this.
Our digestive tract is our main pathway to remove toxins from the body, so daily bowel movements are imperative in ensuring that waste and toxics stuff is excreted efficiently. This is really important for the skin and interestingly, a common complaint often identified in clinic is constipation, or passing fewer than one full stool per day.
A sluggish bowel can result in the recirculation of waste, excess hormones and toxins back into the blood stream (1) and this isn’t good news for our complexion. Our body attempts to find an alternative modality of elimination, which can often be through the pores. In practice, clients often present with spots they identify as ‘under the skin’ when there may be a detoxification or elimination problem. So when your digestion seems sluggish, that’s when pimples can pop up and say ‘hey’! As well as being a contributing factor in acne, lack of daily bowel movement has shown to have an impact on body odour, sweating, brain fog and energy levels.
Psoriasis and gut health
Psoriasis is identified as an inflammatory autoimmune condition – characterised by inflamed, red rashes and patches of skin. The affected areas, which can be anywhere on the body, are often covered with loose, silver-coloured scales which in severe cases can crack and bleed. It can be extremely persistent, hard to manage and fluctuate enormously without any indication as to why which leaves many feeling like medication is their only option...
If this sounds like you, it might be worth giving the gut some attention because as we have mentioned already, 70% of the immune system is created and located in the gut microbiome, therefore having a significant impact on the auto-immune component of Psoriasis.
Though we hate to say it because we LOVE bread, the auto-immune aspect of psoriasis, in some people, can be worsened by intake of gluten, with a strong correlation between coeliac disease and psoriasis. Gluten is the protein found in in wheat, rye, and barley that can't be digested by people with coeliac disease. If you have coeliac disease, your small intestine can be damaged and not be able to absorb nutrients properly which happens due to autoimmune conditions, just like those that can lead to psoriasis. Don’t expect immediate results if you give it up, you need to give it 3 months and also work to support the gut at the same time to see results (more on that below).
Psoriasis and inflammatory bowel diseases (IBD) such as Crohn's disease or ulcerative colitis (UC) can also be linked. In Crohn's disease, any part of the stomach or intestines may be affected; in UC, the lower portions of the GI tract, including the colon and rectum, are usually affected. This is useful when looking to understand where symptoms are originating from and recently scientists have discovered that similar genes may contribute to psoriasis, Crohn's, and Ulcerative Colitis, by altering the structure of some genes (6). Whether or not you have IDB or even IBS, there are also similar mechanisms that trigger inflammation in psoriasis, so it’s still worth giving this organ some support.
Since your skin and your intestines are both made up of tissue that is capable of absorbing things more easily, it's no wonder that both are sensitive to inflammation signals that travel throughout your body and respond to them when they are present. Wondering what to do about this? Skip to the bottom of this article for support.
Eczema and the gut
In similar ways to psoriasis, eczema is characterised with inflamed, red rashes and patches of the skin – which can often develop in childhood. However, unlike Psoriasis, these patches can affect the ‘inner’ areas of the body such as the inner arm, groin, behind the knees and around the eye. All these areas should have natural lubrication from natural bodily oils and sebum production but with eczema this doesn’t happens properly.
It is well documented that the 12 major food allergens play a role in the development of Atopic Eczema, especially since the condition is associated with the dysfunction of the immune system (3) which we know is regulated and controlled by the gut microbiome. If not supported, this inflammation can lead to an inability to regulate the gut flora and an increase in gut permeability (affectionately known as ‘leaky gut’). This creates low-grade inflammation because foods and compounds we consume, can escape into the circulation where they normally would be stopped by the gut barrier. These can then lead to inflammation within the immune system because they shouldn’t be there.
Rosacea and the gut
An imbalanced microbiome may also be a contributing factor towards rosacea and supporting this can reduce the symptoms (7). One study also showed that small intestinal bowel overgrowth (also known as SIBO - an imbalance in the microflora found in the small intestine) is 10 times more prevalent in those suffering with acne than in healthy controls (8). There is also a link between poor digestion of food and an inability to breakdown our food and rosacea, though more research is needed here.
We’ll cover how to address all of this below.
Could my gut issues be linked to my skin problems?
So though we aren’t saying your gut is the only place to focus if you’ve got a skin problem, there definitely is a link between how our gut bacteria can contribute to the appearance of the skin and how common skin conditions are interlinked with our digestive function.
Maintaining a healthy balance of beneficial ‘good’ bacteria in the digestive tract helps to support the microbiome which is vital for keeping our inflammatory response regulated and our digestive function optimal. When there are too few or too many bacteria in the colon, this results in a disturbed ecosystem that in turn may increase inflammation.
How can I manage my gut to improve my skin?
We can think of our gut microbiome as a garden. Having laid the foundations (the soil) for a healthy gut, we can begin feeding and nurturing it (watering it) to help it flourish and perform at its best. Pre and Probiotics are the sunlight and the water to our garden as they feed our gut bacteria, having a significant effect on balancing your microflora.
- Pre and Probiotics:
Eczema sufferers may benefit from probiotic intake, and one study found that those supplementing with a strain of Lactobacillus saw 52% reduction in symptom severity (9). In addition to this, research has found that people with acne tend to have higher levels of the less favourable gut bacteria such as E-coli, and lower levels of beneficial Bifidobacteria and Lactobacillus (10), so it makes good sense to focus on supporting the gut with good bacteria, as part of the management of spot prone skin.
Prebiotic foods such as Onions, leeks, asparagus, carrots, peppers and sweet potato are rich in prebiotic soluble fibre that set the foundations, whilst fermented foods such as sauerkraut, kimchi, miso and tempeh, are all fantastic sources of probiotic to feed the soil.
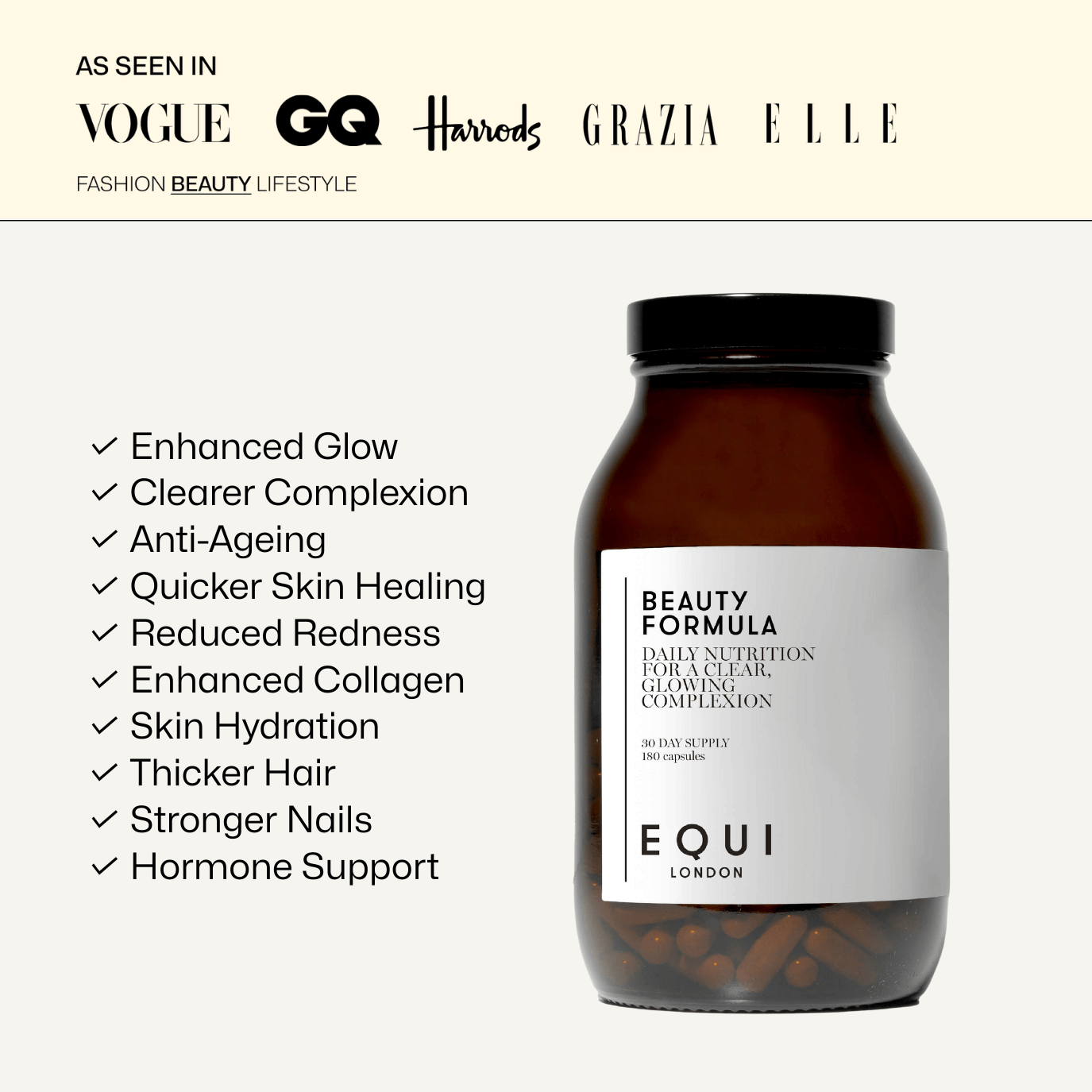
A daily serving of probiotic-rich foods can significantly impact gut health, according to research. Consuming a high-quality probiotic supplement can also be really supportive especially one containing a blend of Lactobacillus and Bifidobacterium, as found in Equi’s Beauty Formula.
- Gut barrier support
We mentioned leaky gut, which might be an underlying factor with all sorts of inflammatory skin conditions. The best way to address this is to cut back on the offending culprits – alcohol, processed carbs, gluten, burnt foods and also be aware of your exposure to NSAID pain killers, never taking these on an empty stomach. Regularly consume collagen rich foods such as bone broth, gelatine and slow cooked joints of meat. Glutamine, turmeric, probiotics and collagen supplements also help to repair the gut lining, and all of these are found in Equi’s Beauty Formula, which is why so many of our customers find it helps with stubborn skin issues.
- Stress
Stress causes a chemical response in your body that makes your skin more sensitive and reactive. In addition, it can make it harder for skin problems to heal and it can flare up gut issues for many people, which is why you may have noticed that you break out more when you’re stressed.
Stress causes your body to produce hormones such as cortisol, which cause the glands on your skin to produce more oil. Acne and other skin problems are more likely to occur on oily skin. Although it is easier said than done, limiting stress and finding ways of management can reduce the severity of breakouts as well as regulating sleep.
- Diet
Regular indulgence of highly processed foods (UHPF) that contain sugar, saturated/trans fats with little nutrient value can often lead to dull, tired looking skin. These can also degrade our collagen production and cause inflammation in the body, contributing to skin complaints.
The aim with skin health is utilising a diet rich in antioxidants, amino acids and collagen, complimenting it with healthy fats that act as an internal moisturiser (think Mediterranean diet!) because all of these are vital for building and rejuvenating our skin.
Omega 3 can also help to reduce inflammation whilst also hydrating skin cells, something that is especially important for eczema and psoriasis. Eat fish x3 week, and include walnuts, flaxseed, hempseed and other healthy fats like avocado and almonds. Our Beauty Oil Edition helps here too turbocharge our Beauty Formula because it contains omega 3 as well as powerhouse anti-oxidant astaxanthin, which has been shown to hydrate and nourish skin cells from the inside out, whilst providing more 'cushioning' between them, creating a smoother complexion 💜
REFERENCES:
- Andrews, C. and Storr, M., 2011. The pathophysiology of chronic constipation.Canadian Journal of Gastroenterology, 25(suppl b), pp.16B-21B.
- De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B and Callewaert C 2021 Gut–Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin ConditionsMicroorganisms9 353 Online: http://dx.doi.org/10.3390/microorganisms9020353
- Katta R, Schlichte M. Diet and dermatitis: food triggers. J Clin Aesthet Dermatol. 2014 Mar;7(3):30
- Salem I, Ramser A, Isham N, Ghannoum MA. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front Microbiol. 2018 Jul 10;9:1459. doi: 10.3389/fmicb.2018.01459. PMID: 30042740; PMCID: PMC6048199.
- Fu Y, Lee C, Chi C. Association of Psoriasis With Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. JAMA Dermatol.2018;154(12):1417–1423. doi:10.1001/jamadermatol.2018.3631
- PMID: 24688624; PMCID: PMC3970830
- Parodi A, Paolino S, Greco A, Drago F, Mansi C, Rebora A, Parodi A, Savarino V. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008 Jul;6(7):759-64.
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future?. Gut Pathog. 2011;3(1):1.
- Drago L, Iemoli E, Rodighiero V, Nicola L, De Vecchi E, Piconi S. Effects of Lactobacillus salivarius LS01 (DSM 22775) treatment on adult atopic dermatitis: a randomized placebo-controlled study. Int J Immunopathol Pharmacol. 2011 Oct-Dec;24(4):1037-48.
- Yan HM, Zhao HJ, Guo DY, Zhu PQ, Zhang CL, Jiang W. Gut microbiota alterations in moderate to severe acne vulgaris patients. J Dermatol. 2018 Oct;45(10):1166-1171.